It's been 4 weeks and I am still loving my results. :) Time has been flying as well! I can't believe its been a month.
I have been about to resume running (approx 2 miles at a time and then some walking afterwards) and I am working on my regular routine of push ups. It still feels weird working chest muscles because I can feel my pecs tighten around the implant. It's a bizarre feeling... not painful... just weird.
Below are my 1 week to 4 week comparison photos. You can see some pretty decent changes, but remember, it will be another 2 MONTHS before they really settle into their pockets and a total of 6 MONTHS before they are all soft and real feeling again.
But the wait is worth it! :)
LEFT Column: 1 Week pics and RIGHT Column: 4 Week pics
As you can see, the right one is a little ahead of dropping than the left, but they'll even out during the healing process.
Next Update will be 07/31/2012 (5 week update and Dr appt)
This blog is about my personal and open experience in having a breast augmentation. The purpose is to help others considering or going through the process to see what my experiences are and to know that they are not alone. Please feel free to write to me with any questions! :)
Wednesday, July 25, 2012
Friday, July 20, 2012
Q&A: When Is The Best Time of Year to Do Your BA?
I had a question emailed to me asking me if I had the choice of the time of year to do have a BA, when do I think is the best time of year.
Well, it depends on where you live.
If you live in a place that has all four distinct seasons (spring, summer, fall, winter) I think the best choice would be a time of year that you can wear looser clothing and things that help to cover you up a little more.
So, depending on your climate, that will vary.
I live in Chicago, IL. We usually have distinct four seasons. Due to upcoming activities for my career, I had to get my surgery now to be healed before I have more physical demands at work. So I really didn't have much choice... I had to do it by the end of June.
But, that being said... I would have liked to have done my surgery in October/November. The reasons being:
- Being hot and uncomfortable sucks.
- Hot = sweaty and sweaty in the summer when you can't shower for a few days after surgery AND if you have your incisions in your armpits you can't wear deodorant for about a week = ew.
- It was hard to find comfy yet normal looking clothing to wear right after surgery and in public for those first few days to a week.
- Cooler weather would have allowed me a better variety of looser long sleeved t-shirts and/or hoodies.
- Summer surgeries limited summer fun. If you want to do specific things at a specific time of year, be sure to plan accordingly. It really depends on what seasons you are most active.
I hope this helps! :-)
Well, it depends on where you live.
If you live in a place that has all four distinct seasons (spring, summer, fall, winter) I think the best choice would be a time of year that you can wear looser clothing and things that help to cover you up a little more.
So, depending on your climate, that will vary.
I live in Chicago, IL. We usually have distinct four seasons. Due to upcoming activities for my career, I had to get my surgery now to be healed before I have more physical demands at work. So I really didn't have much choice... I had to do it by the end of June.
But, that being said... I would have liked to have done my surgery in October/November. The reasons being:
- Being hot and uncomfortable sucks.
- Hot = sweaty and sweaty in the summer when you can't shower for a few days after surgery AND if you have your incisions in your armpits you can't wear deodorant for about a week = ew.
- It was hard to find comfy yet normal looking clothing to wear right after surgery and in public for those first few days to a week.
- Cooler weather would have allowed me a better variety of looser long sleeved t-shirts and/or hoodies.
- Summer surgeries limited summer fun. If you want to do specific things at a specific time of year, be sure to plan accordingly. It really depends on what seasons you are most active.
I hope this helps! :-)
Thursday, July 19, 2012
3 Week Update and Photos 07/16/2012
I've made it 3 weeks past surgery and things keep getting better. :)
My breasts are really starting to feel like my own now. I'm not so consciously aware that they are there and that they are not made from my own body. Plus they continue to soften and become more natural shaped each week. They are slowly losing that angular look and getting natural rounded edges.
I've been wearing the breast strap on them for the last week and I think it's helping.
That plus now that they aren't so firm, it's easier to massage them and the scar tissue around my incisions.
I can comfortably sleep on my sides but sleeping on my stomach does not feel great yet. I don't like the feeling of them under me yet. It's not painful.... It's just uncomfortable.
The doctor gave me the go-ahead to start aerobic exercise again. I plan on starting to jog again tonight and see how that feels and go from there. I'm a pretty active person (yoga, running, lifting weights, swimming, walking, etc) so it'll feel good to get back into a normal routine.
My PS said to just do what feels good and if it hurts, ease back or stop. Which makes perfect sense.
Below are my picture updates. The left column are my 1 week pics and to the right are my 3 week pics. Beneath that are current pictures of my incision scars. They too are SO much better and each week are getting less and less noticeable.
The changes are subtle but they are there. And it's a realistic portrayal of the fact that it does take time to heal up.
Remember... healing and achieving result from your BA is not an overnight thing so be patient. :)
Wednesday, July 18, 2012
2 Week Follow Up Appointment 07/09/2012
I went to my 2 week follow up appointment on 07/09/2012.
My PS was very pleased with the results however to speed up the dropping, he told me it's time to wear the strap to help them drop faster.
This is incredibly common and I was not surprised to hear the news that it's time to strap up.
Veronique Breast Augmentation 3" Strap
The doctor told me to "wear it as much as I can". So unless I am out in public (being that it's summer, it is hard to hide under clothes) I have been wearing it around the house and to bed.
From reading a lot of forums and other women's personal accounts, a lot of women complain about the strap and claim it it uncomfortable or hurts. I find it to be more of a mild annoyance but neither uncomfortable or painful. It is just more annoying to have on than anything else.
I also addressed the "lumps" I had in my armpits near where he cut me open. He said its scar tissue and I am now able to massage it and the scars under my arms to help the lump and sensitivity to go away.
One of the "issues" which I had was my left armpit scar as well. It was very lumpy and rather gross. He said to massage it and it should go down and away on its own. HOWEVER... he did say that if it did not disappear or if I was not happy with it, he will surgically remove it.
I am hoping that with massaging it that it will go away on its own. And it does look better. A 3 week picture will be posted soon showing the healing of my scars.
The doctor wants to see me again in 3 more weeks. So I will have a 5 week appointment with him on 07/30/2012.
Saturday, July 7, 2012
1.5 Week Update with PICTURE Update
I decided to do an update today because of how I am feeling.
It's been 11 days since surgery and today, I actually feel normal! Woohoo!
When I got up, I hopped out of bed, showered and got dressed and realized something was missing.... DISCOMFORT! Yes! Finally!
I noticed when I was doing my normal things, that it was feeling normal. This, to me is a big deal and it will be to you. There is a light at the end of the tunnel and its coming quick.
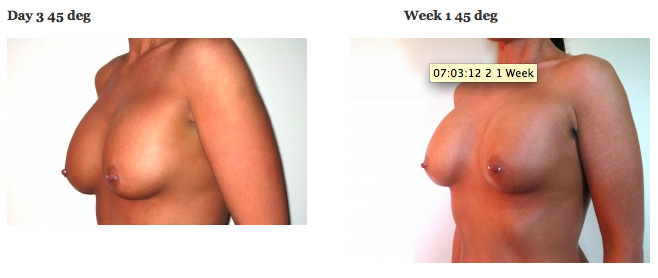
I also decided to take some new pics and compare with my 1 week pics... Especially since there was so much change between 3 days and 1 week. I will still take 2 week pics and post, but the image below shows Day 3 and 1.5 weeks. There are improvements and good changes. More to come!
Plus, they are starting to soften and move a little bit... they are not the solid rocks that they were for the first few days. I am really excited to see what Tuesday (my 2 week mark) will bring. :)
You can see in the 1.5 Wk pics that:
My left breast is still a little more swollen and sitting slightly higher up (which is normal and can happen... the breasts can heal at different rates, de-swell, and drop at different rates).
Both of my nipples are starting to point more forward and look lifted up.
There is a marked roundness starting to show along the bottom and sides of the breasts.
The sloping of the breast from the collarbone down is starting to slide down and not be as angular as is was at Day 3.
It will continue to get better each day. I am excited!!
More to come soon!
Thursday, July 5, 2012
Days 3 - 7 (06/29 - 07/02/12) and PICTURE Updates (3 day and 1 wk Photos)
You will see Day 3 pics and 1 week pics at the end of this page...
And you NEED to look forward to that 1 week mark.... It's a HUGE milestone!
I read and was told that the first 3 days are the worse and then things start to slowly get better.
This is THE TRUTH!
If you are reading this and you are in your first 3 days, hang in there!!
And
remember, your doctor DOES NOT HEAL YOU! He helps your body the best
he can prepare to heal itself. You HAVE to listen to your doctor,
listen to your body and help yourself
to heal up. That plus TIME is
what heals you.
I slept on the couch for the first two nights, but that proved to be uncomfortable. I could see swelling in the small of my back and neither ice nor heat immediately helped the swelling and over all aches I was having in my body.
I
ended up moving to our bed. That felt great! I slept better and with a
lot more comfort. My fiance and I have a Tempurpedic bed and it proved
to be perfect. I still slept on my back, propped up and at a 45 degree
angle but my body and muscles were at least happier.
Taking Care of My Self (With My Fiance's Help) and Following The Doctor's Orders:
I was NEVER in true pain from minute 1 until now. EVER. And the reason why I believe this is because I followed my doctor's orders and took care of myself! I also know that pain tolerance is a player in this too, but you do not have to be Super Woman. Just be Healthy Woman and Smart Woman!
Take
the pain meds as directed to PREVENT the pain. Don't wait until its
already there. I only needed Vicodin for 7 days. That's it.
YES.... In my MIND, it killed me not to be active and moving around. But I listened to my BODY and TRUSTED that my doctor knows best.
Quick Look at Days 1-3 of Personal Care:
-
I took it easy and relaxed a lot! Calming the body and giving it
plenty of fluids and rest helps it to heal! Plus, you will want to nap
often... the pain meds and anesthesia still leaving your body can cause
this to happen too.
- Ice my breasts for 20 min on, 40 minutes off from when I woke up, until when I went to sleep
-
Drank a ton of water, caffeine free diet green tea, small sips on
Ginger Ale if I felt a little nauseous or needed a little sugar
- Took my pain meds and muscle relaxers on time and as directed with water and a few crackers
- Resumed my multivitamin and vitamin c tabs
-
Kept my diet limited to healthy items (plain grilled chicken, dark
green veggies, water, the occasional sugar free Popsicle or frozen fruit
bars
- No caffeine, no excess sugar or sweets, no smoking, no drinking alcohol, and no strenuous activities
- No shower (until the pain pump was removed... My fiance helped with sponge bathing me)
- No laying flat down or on anything besides my back
- No lifting or doing much more than the bare minimum
-
Walking around the house for 5-10 minutes every 1.5 hours (or whenever I
had to get up to pee) to get the blood flowing and muscles moving
Water Is Your Best Friend:
Drink a lot of water! It will help flush out your system and help to avoid bloating! Avoid caffeine and sugar too.
Loss of Appetite But a Fear of Weight Gain:
I
kept reading about all these women who claim the gained actual weight
and looked "pregnant" (due to bloating). This does not happen to
everyone! I fully believe if you are a healthy woman to start and you
are careful and still treat your body well during healing, you will have
NO problems.
Pain
killers also kill your appetite (the pain killers plus not eating
normally also lead to the constipation), which makes matters hard
because you need good nutrients to help you heal. You have to eat
healthy things. It is hard, but you can ration out your intake easily
by taking small bites of good foods throughout the day. It might take
you an entire afternoon to eat the equivalent of a meal, but you need to
keep yourself healthy.
In addition, weigh yourself the morning of surgery. And then DO NOT do it again until you hit the 2 week mark!
Your
body just underwent major surgery. You will have fluid build up in
your breasts and in your body (plus the added weight of your breasts
which out vary from a pound to more, depending on saline/silicone and
size), you may retain some water (and this sounds odd, but drinking more
water will help to flush that out), and, as gross as this sounds, you
will be constipated and after a few good BM's, it will at VERY least
help you to feel lighter.
Bloating:
Again,
I kept reading all these horror stories of women claiming the bloated
up and looked 2-4 months pregnant. I do not know how healthy they were
to start with and how they treated their bodies during the first few
critical days of healing but I did not experience anything even remotely
that bad.
Yes,
I did notice marked swelling around the small of my back for 2 days
(that went away with the help of ice, moving from the couch to my own
bed, and short walks around the house several times a day).
I
also noticed a little bloating in my lower abdomen, but it was very
very minor. And I do think some of it had to do with the fact that I
wasn't standing and carrying myself like I usually do because of the
soreness, pressure, and tightness of my chest and upper body. You know
what I mean... when you slouch or totally relax your muscles, your body
shape in your core can look more puffy than when you are standing or
sitting upright and holding those muscles tighter.
This
look and feeling lasted maybe Weds, Thurs, and a little into Friday.
But, with the little walks, drinking plenty of fluids, removing the pain
pump, starting to be able to hold myself upright (you won't believe how
hard it is to contract muscles around your chest, armpits, and core at
first) I started to look and feel more normal.
And,
as gross as this may sound, after taking a few good healthy BM's, any
worry or look of bloating dissipated by Sunday (5 days after surgery).
So don't freak that you will terrifying. Just BE HEALTHY
and listen to your body. If you are not a healthy person now, I would
suggest getting healthier prior to your surgery. It will only HELP you!
Constipation:
It
took me until Saturday to actually produce a BM (bowel movement). My
last BM was the night before surgery... So I went 5 days! I started to
take Peri-Colace on my 3rd night (Thursday) and took it as directed for
two days. Even with that, it still took 2 days for it to work and help
me out! I finally had a few healthy BM's by Saturday. By Sunday, I felt
"cleared out", lighter and happier.
Incisions: (3 Day and 1 Week Pics below... be prepared!)
My
incisions are under my armpits (transaxillary) stitched with dissolving
stitches, and covered by surgical tape. At my post op appointment, the
nurse told me that I need to leave the tape on for at least 3 days and
after I take out the pain pump and shower, I can let them come off in
the shower.
She did add that the tape MAY come off on its own sooner
and that is ok.
Well, the tape sweated off all on its own by Thursday. And I was not expecting the incisions to look like they did.
Now,
I was warned that the incisions could look puffy and rather gross for
awhile while the skin and nerves heal up. But I was rather taken back
on how gross my one incision looked. (And it doesn't help that you
can't shave your armpits for awhile... probably about 2 weeks due to the
soreness and the incision! So gross!)
Prepare yourself.... These are kinda gross.
And yes, the images have been blurred some... I blurred out the armpit hair... It make the pic even more gross, I hate body hair, and it is just icing on the cake of gross. LOL.
LEFT Armpit Incision 3 day Mark 06/29/12
RIGHT Armpit Incision 3 day Mark 06/29/12
Yes, there is some bruising, but it is mild. And that is the ONLY bruising I have, even now, 1 week later.
1 Week Armpit Incisions
Yes... still can't shave... and yes, it blurred that out. Ew.
LEFT Armpit Incision 1 Week Mark 07/02/12
LEFT Armpit Incision 1 Week Mark 07/02/12
As you can see, minus the blurred out armpit stubble, the incision scars are looking better.
Removing the Pain Pump: http://youtu.be/SCkMCICEZpY
The
above Youtube link is NOT me, however it will give you an idea of what
its like and what to expect. Beware... it could make your a little
queasy.
My doctor told me that when the pain pump runs out in about 3 days and I can go ahead and remove it myself.
The directions were as follows:
-
When the pain pump is empty (all the juice is gone and there is just a
hard small cylinder in the middle of the clear plastic bag with the On Q
written on it) it is time for removal.
- Carefully pull of the surgical tape holding the tubes in place.
- Place your fingers as close to the tube entry near your skin and slowly start to pull the tube out
- Repeat on the other side
He said not to worry, there will be no pain but I might feel the tubes moving and sliding out from inside my breasts.
He also warned that there could be a drop or two of blood by the entry site and have a tissue or gauge ready.
Well,
it was removal time and I was grossed out and queasy at the whole
idea. My fiance helped out though and made it easier for me.
Removing the tape was the only painful part. That stuff is on there like glue!!
Once
the tape was off, he started to pull the tube. It felt like he was
pulling forever and I 100% felt that tube sliding around in my breast.
It was rather freaky! It DID NOT hurt, but was just such a crazy gross feeling.
After
he got the second tube he showed me how much was actually inside me....
The better part of 8 inches of tube in each breast! Crazy!
I did feel a lot better after the pain pump was removed but I really think it was all psychosomatic...
The idea in my mind that the removal of the pump was a sign of getting better, not needing it and moving on with healing. That, and it felt so good to not have to wear the fanny pack, carry the pump around, having all those tubes taped to me and risking getting caught near the fanny pack, etc.
Either way, by Friday afternoon, I noticed a HUGE improvement on how I felt!
But, I am GLAD I got the pain pump. I HIGHLY
suggest it! I do not know how I would've felt without it, but
considering I was never in real pain, I am guessing it had something to
do with making that happen.
Wow... This is real and this sucks! It was something I read about and I was prepared for just in case.
And I am glad I did.
Here is how I felt following and when it hit me...
The
moment the bandages came off I was rather apathetic to the look.... I
was neither excited nor upset because I knew going into it that it was
not going to look like the final product and that I have at least 3
months before they get more normal. So I was ready for the "great
unveiling".
But after I got home and things settled down and I realized how weak and sore I really was, I started thinking.
When
I could barely pull my own shorts up, couldn't open the fridge door,
couldn't shower, stuck inside resting, couldn't shave or wear
deodorant... My breasts were so swollen, hard, and tight. I felt like I
got hit in the chest by a baseball bat, my body felt swollen and my
body ached, and I started to really wonder if I did the right thing....
That's when I looked down at myself and thought, "What did I do?? I "disfigured' and maimed myself!"
I felt like I'll never be able to go for a run, lift weights, do push ups, or even hug anyone normally!
When
I looked down I just saw these two huge massive breasts that jutted out
so far, looked uneven and hard and on top of it, I felt like EVERYONE
who looked at me would see these and know they were fake. I even said
at one point that I wish I had never had the surgery.
I felt unattractive, disfigured, grotesque, weak.... and I felt ashamed to show my body to my fiance.
He
was wonderful through it though. He did his best to make me feel good
and told me how good everything is looking. He reminded me that what I
am feeling is normal and it will get better.
It took until about Monday (6 days after the operation) to start to feel better about how I look and feel.
But
once I started to feel better, the tightness and soreness started to go
away and when I started to feel more like myself, things started to
perk up.
I now am over the post-op blues and I know that over the next few weeks and months, things WILL continue to get better.
Hang in there... you WILL feel better!!
Exercise:
My
doctor said after 3 days, I can start to resume light exercise, like
take 30 minute walks a few times a day to start. And I was walking by
Saturday. That really helped to make me feel better. I have been
walking 30-60 minutes every day since.
The first few walks I did feel tight and it was uncomfortable. But each day, that gets better too!
I also have resumed doing normal things at home, with caution. I have been able to do laundry, cook, clean, etc.
It also makes you feel better to get back into a normal routine.
Sleep:
Sleeping has been... interesting....
Now
that I am feeling better, during the night, my body keeps trying to
turn over onto my side to sleep. I still have my pillows on either side
of me that keep me from flipping totally over and also help to support
my breasts if I do turn. It has seemed to help too.
The following are 3 day pictures and 1 week pictures for comparison. It's getting better!
Next update will be the 2 week mark on 07/09/2012
Removing the Pain Pump (6/28/12)
Removing the Pain Pump: http://youtu.be/SCkMCICEZpY
The
above Youtube link is NOT me, however it will give you an idea of what
its like and what to expect. Beware... it could make your a little
queasy.
My doctor told me that when the pain pump runs out in about 3 days and I can go ahead and remove it myself.
The directions were as follows:
-
When the pain pump is empty (all the juice is gone and there is just a
hard small cylinder in the middle of the clear plastic bag with the On Q
written on it) it is time for removal.
- Carefully pull of the surgical tape holding the tubes in place.
- Place your fingers as close to the tube entry near your skin and slowly start to pull the tube out
- Repeat on the other side
He said not to worry, there will be no pain but I might feel the tubes moving and sliding out from inside my breasts.
He also warned that there could be a drop or two of blood by the entry site and have a tissue or gauge ready.
Well,
it was removal time and I was grossed out and queasy at the whole
idea. My fiance helped out though and made it easier for me.
Removing the tape was the only painful part. That stuff is on there like glue!!
Once
the tape was off, he started to pull the tube. It felt like he was
pulling forever and I 100% felt that tube sliding around in my breast.
It was rather freaky! It DID NOT hurt, but was just such a crazy gross feeling.
After
he got the second tube he showed me how much was actually inside me....
The better part of 8 inches of tube in each breast! Crazy!
I did feel a lot better after the pain pump was removed but I really think it was all psychosomatic... The idea in my mind that the removal of the pump was a sign of getting better, not needing it and moving on with healing. That, and it felt so good to not have to wear the fanny pack, carry the pump around, having all those tubes taped to me and risking getting caught near the fanny pack, etc.
Either way, by Friday afternoon, I noticed a HUGE improvement on how I felt!
The Post-Op Blues; It’s Real, It Sucks, But It’s TEMPORARY
The Post Op Blues (or Post Operative Blues) can be described as:
A short episode of mild depression is actually not rare after cosmetic surgery of any kind, breast augmentation included. It may last from a few days to several weeks, and is in many ways similar to the “Baby Blues”, known as postpartum depression, that can occur after labor and delivery.
There are many things that can contribute to this brief mild depression, and it is likely that several factors are present in combination, to different degrees depending upon the individual circumstances.
Here are some factors that can contribute to “Postoperative Blues”:
1. Sometimes a person may be so excited about their upcoming surgery that they have a sort of giddy euphoria about it. One aspect of this feeling is actually chemical – substances like steroids, adrenaline, or endorphins produced by the body. After operation, these chemicals stop, and there is a sort of let down. This is similar to what happens after childbirth.
2. Sometime the woman may have been hoping that having breast augmentation would change her life or her relationships. Reputable plastic surgeons do everything they can to clear up such a misconception before ever scheduling the surgery, but it can still happen nevertheless. Breast augmentation will not improve a failing relationship.
3. Some surgeons do not properly involve the patient in the size decision, giving the patient little or no input into the process. Or worse, some surgeons impose their own tastes or preferences upon the patient, deciding for them what size they should be. These approaches do not work and will likely leave the patient feeling that after all the trouble and expense she is the wrong size.
4. Many women have a natural tendency to feel guilty when they do something for themselves, particularly if it means spending money on their appearance, when the funds could have been used for other purposes.
5. Many people habitually compare themselves to others who are less fortunate, and then feel guilty or vain for spending money on themselves when they know that there are people starving somewhere. People who have this viewpoint have difficulty accepting any of the good that they have in their own life.
6. Certain religions encourage people to feel guilty about doing things for themselves. Other religions do not permit people to electively choose to change any physical aspect of their bodies. Even if a religion is not that extreme, it can still make the woman feel uneasy on vaguely religious grounds.
These are just some of the factors, and several may be working together. But don’t worry, it is normal, and usually temporary.
It is something that CAN happen
and YES, it happened to me.
You will see it referred to in the posts
during the few days after surgery.
But remember, THIS TOO WILL PASS!!
Wednesday, July 4, 2012
Day Two/Second Night After Surgery
********************
Written at 10pm on 06/27/2012, 31 hours after my surgery
********************
The car ride home was incredibly uncomfortable but I was very happy to get home.
I got all set up on the couch propped up, took my next round of meds and dozed on and off all afternoon. I've been able to pee without any issues, but still no BM. I think if I was able to poo I would feel better. :(
I've also been icing my breasts often and I think it's helping. But the weight of the ice can sometimes be uncomfortable. And I've been keeping up on using the breathing toy to keep taking deep breathes.
I've noticed my breasts and body is feeling slightly itchy too. But I can't always reach the right spot. :( So my fiancé gave me a chopstick for scratching stuff. LOL
The doctor prescribed me a medication to help me sleep tonight and for the next few nights. I hope that will help.
Other than that, it was a decent first full day and second night I think. Even though I am currently just not feeling "right". I'm hoping that the next few will be even better.
It's the better part of 90 degrees out still with a high of 100-110 with the heat index tomorrow. So unless it cools off some, I'm going to hold off on that walk. Those temps and no shower or deodorant = gross.
Here's hoping for a good night's rest.
More tomorrow. :)
Update: It's 4:23am and I'm due fur my next pain pill at 4:30. I think my body is pretty in tune with what I need and when.
From around 12a until now, I've slept soundly and when I awoke, I peed and it wasn't too bad moving. Comparably speaking that is.
More to follow.
Labels:
ice,
icing,
itchy,
medication,
pain pills,
Second day,
sleep,
sore,
tight
Post Op Appointment 06/27/2012 @ 10am
********************
Written at 4pm on 06/27/2012, 25 hours after my surgery
********************
First of all, after a pretty decent first night, I was very sore when I got up this morning. My whole body was tense, tender, and achy from head to toe.
Part of the tenderness was from trying to stay propped up all night. Some was from trying to hold still and not jostle myself around. And of course, some of it was from the overall trauma on the body caused by surgery and my body trying to start healing.
My fiancé helped me again this morning get cleaned up (I cannot shower yet) and dressed (I still cannot move about freely without mass discomfort).
I was a little grouchy to him though and I feel bad about this fact. I think it's a combo of not sleeping soundly, the pain meds, and being so uncomfortable.
I can say this as a 100% truth... Words cannot describe how glad I am that I have a pain pump and stayed close to my doctor's office.
I still will not call what I feel constantly as "pain". It is still just a tightness and overall soreness with a little pinching under the arm put near my incisions.
But, again, I have a pain pump and I am taking my pain meds, antibiotics, and muscle relaxers around the clock as prescribed by my doctor. I also follow each pill time with a few whole wheat saltines and have not felt nauseous. I am not really hungry though.
I am also continually drinking fluids (Gatorade, water, Crystal Light, ginger ale) and today I resumed my Once a Day Vitamins plus Immunity Support Gummies (my body seems to tolerate these better than other OTC vitamins) and 2x a day Ester-C 1000mg Vitamin C pills.
I cannot say if the two vitamins are helping more at this point yet but my doctor did suggest taking them prior to and after surgery. And he has been right so far.
After he got my cleaned up and dressed, we checked out of the hotel and got in the car. The walk actually felt decent after I got stretched out some.
The car ride was a different story. I felt every bump, dip, acceleration, brake, sway, curve, slight elevation change, etc. And my fiancé was so careful driving. He couldn't have been any more cautious.
We got to the doctor's office and I was immediately brought into an examination room. The nurse asked me a few questions and after I gave her the good news on my "pain" level and how I was feeling she told me I was about to feel better.
She had me remove my hoodie and she started to remove the bandages. It was instant pressure relief; like the pressure was reduced by 80%. It wasn't painful, but the weight of the breasts unbound was a weird feeling.
After it was all removed I got my first glimpse of them in the mirror. They did not look as bad as what I was expecting.
From reading other people's stories and the "warnings" from people's experiences and doctor's info, I was expecting the worse. But it wasn't too bad.
They were swollen and looked bigger than what I wanted, but I was expecting that already. The implants were not sitting too high though and they already have a good shape. My nipples were not pointing down or tweaked in any way. The nurse was pleased and so was my fiancé.
She gave me the breast band in case the implants start to ride too high with instructions to call the office before I put in on. She said that I don't need it now but just in case, the doctor wanted me to take it.
The nurse also said that the doctor approved me walking for short, 30 min walks starting today if I feel like it and if I feel like it will help.
The doctor had an emergency that he needed to address so I was unable to see him today. I wasn't thrilled with that but what can ya do? I have faith in his staff and I can always call if I need something.
The nurse said to pull the pain pump out Friday and once it's out, I can shower. She said to be gentle because of the sutures under my armpits and the tape covering them. I guess they'll take up to month to dissolve. But on a positive note, I can wear deodorant starting on Monday or Tuesday.
I asked the nurse how long the incision is but she said she didn't know. And it's too sore to lift my arms to look. That and the tape is covering them.
I made my next appointment with the doctor for July 9th (12 days from now).
Man, I am worried about pulling the pain pump tubes out on Friday....
My First Night Post-Op
********************
Written at 7am on 06/27/2012, 16 hours after my surgery
********************
My wonderful fiancé helped me stay up on icing my breasts and keeping up on all my meds. He was a godsend.
I had no issue peeing through the night either, but I'm not surprised that I haven't produced a #2 yet.
I noticed bleeding from around my pain pump tubes which I'll address with the doctor today.
I'm still not in pain; just the constant pressure and tightness is always present. And there is still the feeling of little pinches from under my armpits.
Moving around is an interesting feeling too. I slept on my back propped up at a 45 degree angle. And my whole body feels sore. I have decently strong core muscles so standing up isn't an issue, but it feels very weird once I'm standing.
My chest feels heavy and standing makes the weight feel more shifted to the front (as opposed to the weight feeling more spread out when I'm reclined). And my shoulders feel like they want to stay in the shrugged position (they are very tight and it's hard to force them to relax).
My back is also tight and feels tweaked from sleeping in such a weird position for me. I'm a side and stomach sleeper so this is all just new and uncomfortable for me.
I'm worried that the combo of the muscle relaxer, pain killer and antibiotic plus the walk to the car, the drive to the doctors office, and the drive home will make me nauseous or worse. So I am planning to take an anti-nausea pill about 8:45am (25 min after the rest of my pills).
Here's hoping it'll help.
Well, it's time to start getting ready to leave the hotel. I'll update the post-op doctor's appointment later today.
Labels:
bleeding,
chest,
first night,
heavy,
hotel,
night,
pain killer,
pain pump,
post surgery,
post-op,
pressure,
sore,
tight,
weird
Surgery Day 06/26/12 @ 1:30pm and Post Op (Bandaged) Photo
********************
Well, I wrote this post a little over 7 hours post surgery. It went well. :)
********************
I woke up about 9:30, showered, washed my hair and scrubbed all over really well with Hibiclens.
At 10:30am, I took Emend (a pill to help with nausea.... When I had my wisdom teeth pulled YEARS ago, it made me violently ill, so the doctor and anesthesiologist planned ahead for me to try to help me not get sick).
By 11:30, I was showered and ready to go. I was also hungry and thirsty. :( I hadn't eaten since 12a and no water since 4a.
The ride there was quiet.... My fiancé held my hand and told me that everything will be just fine. Just his presence made me feel better.
We got to the surgery center, signed in, I signed final paperwork, and was temporarily separated from my fiancé.
The nurse brought to my recovery room and he was asked to wait for a few minutes while they started my process. I put on a gown and silly surgery grippy socks and got comfortable.
The nurse asked me a few final questions, answered my questions and took my vitals. Another nurse who would assist in surgery came in to say hi and see how I was doing. She was sweet, very warm and friendly like the first nurse.
The anesthesiologist came in and helped to calm me. He gave me a pain-free IV and said when I get in the surgery room, he will let me know when the "sleep time" will start.
I had to give a urine sample to the nurse and when I returned, my fiancé and the doctor were waiting for me.
We talked to the doctor. He answered final questions, put me at ease, and marked my chest for surgery. He said I'll be in surgery for 45 minutes to an hour and we will be starting soon.
He left to prepare and within minutes it was time to go. My fiancé kissed me and I was wheeled off on my recovery bed.
In the surgery room I started to get really nervous. But the staff was AMAZING!!
The nurse had me slide from my recovery bed to the surgery bed and got me comfortable. She laid a warm blanket on me and massaging leg wraps on my calves. I had to stretch my arms out and they were covered up with warm towels.
The anesthesiologist told me that it's time to start and to relax. He said I'll close my eyes and when I open them, I'll be in recovery. He did warn me that there would be a chance that I might wake up a little when I am sat up to be bandaged (but I did not).
He said to tell him when I feel something... And about that time I sure felt something. I was able to say "I think I am starting to feel..." and that's all I remember.
About an hour or so later, I started to come around in the recovery room. I was greeted by an incredible recovery nurse. He was the best of them all.
I don't recall too much right away other than having to move from the recovery bed. And I know I felt a little nauseous
The anesthesiologist came in and he and the nurse gave me more meds. The anesthesiologist told me he also gave me a lot of anti-nausea in my IV too.
I was in and out of it for what felt like a long time. My fiancé was the best though! He helped me take sips of water and ginger ale and have me cracker bites.
When I had to focus and do something, I could. But I fell asleep in between those times.
I didn't feel true pain (and now it's 9:46 and I still haven't). My arms sore (the nurse told me its from the way they have to manipulate them during the surgery( and armpits are a little "pinchy" (again my incisions are there and all the gauze and bandages are kinda rubbing me funny).
Otherwise the feeling is a terrible pressure on your chest, the weight and tightness is manageable but is very present. I won't call it pain really.... It's more of an uncomfortable, constant pressure and tightness.
Plus it's taken up till now to be able to take a deep breathe without a great deal of pressure and increased tightness. The nurse gave me a breathing toy where I have to make the ball float in the tube when I breathe in to help me use deep lung breathing.
(Later I realize how much it helps.)
My doctor came in to check on me, have me take a hydrocodone (Vicodin) for pain (even though I wasn't in that bad of pain). He said everything went very well and that they look great. He seems genuinely excited to show me them tomorrow.
He said I still have to pee before they will let me leave and to try to go soon.
The nurse came in and helped me walk to the rest room... And it was a no go.
So I drank a cup of water, a can of ginger ale, and three little cans of cranberry juice (on top of two IV bags I already had running through me..... Guess who was probably dehydrated when she went into surgery...).
The nurse also showed me a few tricks like pouring warm water over the genitals, bare feet on the cold floor, running water, and finally walking laps.
Then he dropped the catheter bomb if I couldn't pee on my own....
I tried one last time and I really strained. I finally peed!!
But the activity and straining made me nauseous!
I returned to the room my fiancé helped me to dress and the nurse gave me Zofran for the nausea. And it took a little bit, but it eventually helped.
The nurse wheeled me out to my car and assisted me in. He was so sweet and comforting. And he commended my fiancé for his excellent care of me. He said that he is hired! :)
Since we don't live close to the doctor's office, we opted to stay at a hotel close by. And I am SO thankful for that!!
The short few mile drive was slightly painful. I really couldn't support myself all that well since I have the armpit incision and the gauze is padded up pretty thick under there.
We finally got to the Hilton and I was wheeled up to the hotel room. I didn't feel nauseous anymore and was just sore.
And I got my first glimpse of my chest. WOW! They already look good and I'm so excited to see them tomorrow. My fiancé seems excited too. :) And he also seems more calm.
My fiancé got my all set up on a bed and comfortable. and we ordered something to eat. I enjoyed a nice fresh caprese salad and I did not feel ill at all. I took my antibiotic and painkiller and had some Gatorade.
I am now resting comfortably, and am going to watch some TV and relax. I'll be taking more painkillers and a muscle relaxer soon. The pain pump seems to be helping too. Not that I have anything to compare it too, but if you're on the fence about it, I would say it's worth it. I wouldn't want to know what it feels like without it.
I will say this though, I am experiencing a little bleeding from the tubes from the pain pump. It's not terrible and doesn't hurt. But it does look a little freaky. http://www.iflo.com/prod_onq_classic.php
My post-op appointment is at 10am on 06/27/2012. I'm excited for that and yes... I'll be updating that appointment and finishing older posts too.
Labels:
Air-Eze,
anesthesia,
anesthesiologist,
cutting,
driving,
emend,
Hibiclens,
Hilton,
hotel,
IV,
nauseous,
numb,
On Q,
operation,
pain pump,
post surgery,
pressure,
recovery bed,
tightness
The Night Before Surgery
The night before surgery was rather stressful for both me and my fiance, even though we had been getting things ready for the last two weeks.
We made hotel reservations; we decided to stay in downtown Chicago the night of the surgery to minimize the drive after surgery and to stay close for the post-op appointment and packed bags for the next day.
We literally cleaned the house from top to bottom, packed a surgery suite bag, and I set up a little recovery “bed” with on the couch in the living room.
The surgery suite bag included:
- all my medications
- the “Patient’s Bible” from my doctor
- paper and pens (in case my fiance had to make notes)
- Chapstick
- Loose mesh workout style pants (in case I was cold)
- Socks and light weight tennis shoes
- A loose zip up hoodie
- A bottle of Gatorade
- 2 cans of Ginger Ale
- 2 small bottles of 7-Up
- A sealed pack of low sodium whole wheat Saltines
- Baggies for ice
- Snacks for my fiance while he waited for me
- A lined puke bag in case I got sick on the drive out of the surgery center
This bag also doubled as the car ride home bag in case I needed anything for quick accessibility.
We brought extra drinks, crackers, and bags into the hotel in case I needed anything.
I also placed a puke bag in the car and one by my make shift recovery bed.
For my recovery bed on the couch I lined he cushions with a soft bed sheet and used a lot of pillows to keep myself propped up (the doctor wanted me sleeping on my back and propped at a 45 degree angle for at least a week if possible). I had extra to place at the small of my back for lumbar support and a few for under my knees and feet if my legs ached. I also had some on either side of my to prop my arms up (picture a throne).
I had another top sheet ready and a super cozy plush blanket in case I got cold. I had a tray on the couch with a Gatorade, a Ginger Ale, my cell phone/iPad/computer charger and crackers so all my fiance had to do when we got home was to help my lay down.
I basically was prepared for when we arrived home, it would be an easy transition.
I also looked at some web pages and found some good tips for the night before surgery and post surgery care ideas:
http://www.implantinfo.com/faqs/1.41.aspx
Week or More Before Breast Implant Surgery
- Keep your doctor in the loop about medications, vitamins, supplements, colds, other issues that may affect your ability to keep your date.
A Few Days Before Breast Augmentation Surgery
- Wash hands religiously. Avoid sick people.
- Arrange a ride to and from surgery and someone to care for you (at least 48 hrs).
- Arrange for child care for two days (minimum). If you have to lift young children, get help for several days.
- Arrange for pet care. Food litter box, etc. Better yet, have someone care for them.
- Head off would-be callers and visitors during your recovery. Do this in advance.
- Fill prescriptions. Buy Neosporin, gauze for changes, vitamins and anything approved or requested by plastic surgeon.
- Shop for / cook some foods in advance (like soup). Have simple foods ready to eat (crackers, soup, Jell-O, canned health drinks) in case you can’t eat.
- Buy 1 or 2 large jogging or sports bras that open in front (no wires) and stretchy comfortable pajamas.
- Get a bell to call your helper during your recovery.
- Pay bills and do your banking
- Recharge / replace batteries in remote, cell phone, cordless phone.
- Set up a table close to you with things you’ll need when you get home: medications, T.V. remote control, phone, vitamins, tissue, books, magazines, water bottle, etc. Keep a plastic waste can nearby (anesthesia and medications can make you nauseous).
The Day Before Surgery
- Do the laundry. Clean the house and do the dishes.
- Gas up your car. Rent 3-day movies. Put favorite one in DVD player.
- Locate button down shirts and stretchy pull-on pants. Set out for easy access
- Consider sleeping on the couch / recliner for the first night or two. Make up couch or chair with sheets, blankets and pillows plus a U-shaped pillow. It feels good to be somewhat upright.
- Make up your bed with fresh sheets and pillows.
- Put dry foods on the counter and refrigerated foods at lower levels to avoid reaching. Loosen jar lids, etc.
- Get a bag of frozen peas, ice bags or frozen gel packs ready for swelling and a heating pad for a sore back.
- Put all of your garbage out. Get a good night’s sleep! If your doctor told you not to eat or drink, DON’T!
The Big Day – Before You Head Off to Surgery
- Take a nice long hot shower and wash your hair. Shave everything before going. No makeup, hairspray, deodorant, powder (nothing!).
- Wear warm socks or slippers for surgery. Have comfortable shoes and baggy clothes and top that buttons in front for dressing after surgery. A men’s dress shirt will do the trick.
- Put post-op checklist near your bedside table with your bell.
- Arrange bathroom – Put toilet paper in reach. Organize items so they are ready to go and to avoid bending and reaching (mouthwash, toothpaste & brush, hair brush, contact lens stuff, makeup, etc.)
- Take a coffee can or something with a lid for the ride home in case you get sick. : (
- Bring cold ginger ale or water to sip on the way back home.
- Bring Chapstick for your lips.
- Have pain medication available (as directed by doctor) for the ride home.
- Remove your contact lenses and switch to glasses if you need to.
- Bring your list of any last minute questions.
http://www.breastimplants4you.com/
- Have your significant other, parent or good friend there to take care of you for the first 48 to 72 hours. It is very important to have someone to wake you for medications, help you to the bathroom, prepare food for you and make sure that you eat it, and to be there in the event of an unforeseen emergency.
- Take your pain medications. There is simply no reason to suffer. Studies have proven that patients who are in pain and have a lot of stress can expect to significantly increase their healing time. Take care of yourself.
- Take your antibiotics on time; you do not want an infection. Finish your entire course and do not skip pills.
- Be sure to follow your surgeon’s advice on icing and be sure to change out the cold packs often. Keeping the area cold can really help diminish the swelling and discomfort, especially in the first 48 hours. Do not place ice or a cold compress directly on skin. If your surgeon says no icing — no icing. Abide by your surgeon’s rules.
- Try to eat something, even if it consists of a few bites. You need your energy, because your body is working overtime to heal itself. Taking medications on an empty stomach can cause nausea and dizziness.
- It is very important to drink plenty of water. Your body needs water to help flush out the residual anesthesia and pain meds, especially after you stop taking them. Plus, your body will retain more fluid if you don’t drink enough water, resulting in more bloat and increased swelling. Also, your medications can cause constipation, and being dehydrated can only make things worse.
- Remember that swelling is normal, as is bloating. If you accept it and continue to drink water and eat a balanced diet, all will subside in its own time with a lot less stress.
- Some patients recommend Daikon (a root vegetable) to help with constipation that is brought on by pain medications. It also helps flush out the system. Daikon may be best after you are finished with your medications. Mild stool softeners like Colace are really effective, but please ask your surgeon first.
- Sleep with your chest elevated for at least 10 days.
- Have pillows alongside of you as well as in back of you to support your arms and assist you in trying to roll over on your stomach or sides. You may wish to add a small pillow at the lower back for sleeping.
- Take your temperature regularly. An elevated temperature could mean an infection.
- Take your antibiotics ON TIME. Don’t forget if you are taking birth control pills that some antibiotics can interfere, so in the event that you do have sex, use another form of protection as well.
- When you get tired, sleep. Sleeping gives your body more time and energy to direct towards healing.
- Get up and walk around when you are able, but don’t overdo it. Too much too soon spells disaster.
- If you were fortunate enough to have quit smoking, please do not start again. Smoking narrows blood vessels and decreases the amount of hemoglobin to the wound. This can result in wound closure problems and necrosis (death) of skin cells and tissue.
- Keep moist towelettes or baby wipes near the bed. These are great for freshening up without much effort.
- Keep the ringer on your phone turned off in your room. A constantly ringing phone will keep you from getting much-needed rest.
- Have a whistle, walkie-talkie or intercom system on hand so that you can alert your caregiver if you need them for any reason.
- Ask your surgeon about silicone gel sheeting, Steri-Strips from 3M, Mederma scar gel or whatever else your surgeon may recommend for helping scars.
- Remember to take your after photos or day-by-day photos if you are keeping track. Have your caretaker take several photos during your recovery. You may not remember having them taken or may even get aggravated with a camera in your face when you don’t feel well, but you will appreciate it later if you are keeping close documentation.
- Remember to write in your journal daily because you will forget later due to the amnesiac properties of the anesthesia. Use a miniature tape recorder to keep track of your experience, if you prefer.
- No walking around without a support garment unless your surgeon specifically told you not to wear one. Your breasts will need support during this time for several reasons: breast shape, scar stretching, pain and trauma to the healing breasts.
- If you have online friends, have someone post or email them after your surgery or they are going to worry about you.
- Make sure you don’t take any products that contain aspirin — and don’t drink any alcohol — for at least two to three weeks after surgery.
- Have your friends stop by when you are feeling better. Get some fresh air if you can; it will do you good. Just don’t overdo it.
- Remember, you will have scars and they will look worse before they look better. Please don’t be depressed because of the scars. Your breasts will continue to change over the next few weeks and months, and the scars will be less visible. The scars are at their reddest in the first three to four months. Depression and stressing out over every little thing is NOT good for proper recovery.
- You shouldn’t ride any roller coasters or other types of amusement park rides. If G forces can cause aortal tears, they can cause internal tearing and bleeding in freshly healing tissues. Also refrain from horseback riding and contact sports for several weeks. Be sure to ask your surgeon when you can continue these activities.
- If you have topical arnica montana gels, take care not to get the product on your incisions. Arnica montana can irritate your wounds and cause inflammation.
- Many surgeons recommend that you continue taking vitamin C during your recovery. Ask your surgeon if he or she approves.
- No lifting objects over 5 to 7 pounds. This includes children and pets.
- No bending over. Bending over increases pressure on your wounds and may cause hemorrhaging. Squat down, if you must, but do be careful. This is why it is important to place things at hip level beforehand or have a caretaker.
- If you suspect you may need to pick things up, perhaps buy a “reacher” marketed for this very purpose.
- No raising your arms way over your head. Ask your surgeon when it is safe to do so.
- One of our visitors suggests tying a long string to the ceiling fan light/fan cords.
- Be careful with your significant other and children, and tell them to be careful. Being hit in the breast after surgery can cause bleeding, suture popping and pain.
- Sleeping upright can cause back cramping. Try hot water bottles or heating pads to alleviate this, but remove them when you sleep as they can cause burns. Also, keep heat away from your breasts unless otherwise instructed.
- Watch for suspicious swelling and discolorations that could be a hematoma. Learn the difference between a hematoma and a bruise.
- Make a chart of when to take your meds or use the med chart we have provided. Some are taken 1 every four hours, some are taken four a day. Don’t confuse the instructions. A pill case will help you keep your medications in order.
- Place a waterproof, non-slip stool or plastic chair in the shower when you are finally allowed to shower.
- After you shower, place a towel on the closed toilet seat and sit down to dry yourself. If you are dizzy from your pain medications, you may fall and hurt yourself.
- If you are expecting your period and it does not come, do not worry. The medications, trauma and anesthesia will probably disrupt your cycle. This goes for it coming at an inopportune time as well, such as surgery day. Just have your feminine supplies on hand and expect it when you least expect it, or not at all.
- You are probably going to be depressed a few days after your surgery or at some point during your recovery. This is very normal. Just warn your loved ones beforehand and keep your chin up. Your body has been put through a trauma, albeit a planned trauma, and will make you pay for it in its own subtle ways. Depression may rear its ugly head with crying sessions, feelings of unattractiveness, self doubt, regret and general sadness. This, too, will pass.
- Do not be afraid to contact your surgeon if you feel there is something wrong. Surgeons are accustomed to talking with patients who have questions or just need reassurance.
- Go to your postoperative appointments. These are important so that your surgeon can gauge your progress and assess any further needs you may have to improve your results or experience. It’s also when you can share your thoughts, express concerns or ask advice.
- Most importantly, relax. Don’t stress. Being stress-free is very important for your recovery
The Two L-O-N-G Weeks Before Surgery
As soon as I walked out of my pre-op appointment, I did what almost all nervous people do before a surgery...
I got on the computer and started researching, read, and in some cases, freaking my self out!
The links I provided in my Welcome/Preface page really helped me. There is a lot of good info in there.
I also started reading about other women's accounts to see what I might expect. This was a double edged sword. It helped because if everyone said that they felt better in X amount of days, then I felt good I might feel good then too. But reading about the darker side of BA's and even though my surgeon already talked to me about all of it, it still made me anxious.
My fiance kept yelling at me to stop because I was just getting myself worked up, but for whatever reason, I couldn't stop.
I started to have anxiety dreams/nightmares. I guess that is pretty common.
I also had an idea of what I MAY expect after surgery and that actually helped.
Things that I prepared myself to (or that I might) experience include but were not limited to:
- Knowing the 1st 3 days after surgery will be the worst
- Post Op blues (please see my post "The Post-Op Blues" specifically on this topic http://ej339cc.wordpress.com/2012/07/04/the-post-op-blues/ )
-My breasts will be extra big and NOT the final/right size due to the swelling for awhile
- They might be sitting too high and may need a band to help pull them down
- My nipples might point down or be uneven for awhile
- I could be bloated for days to a week or two (usually due to anesthesia/pain meds)
- I could be constipated (usually due to anesthesia/pain meds)
- My breast skin could become extremely shiny
- My breasts and/or nipples could be numb and/or hypersensitive
- My incisions could look puffy/natural/pretty gross and produce yellow crust
- My breasts could heal at different rates, drop at different rates, soften at different rates, etc
- Not liking what I see for awhile/feeling unnatural/feeling regret
- What to do to prepare myself and my house for coming home from surgery
So for days before my surgery, I read and read. I do not know if it hurt anything, but I think it helped a lot.
I was also able to better prepare my fiance for what to expect both physically and mentally for me. I know that helped him.
I also got my medications filled and went to the grocery store to be sure I would have everything I need as soon as I got home.
I knew that icing your breasts is a big help and to plan for that I got these cool gel like cooler "sheets". They were light weight and covered my whole chest from armpit to armpit and collarbone to lower ribs.
One of the cool and fun things I did get to do was that I gave my best friend my collection of Victoria's Secret "Miraculous" bras (the ones that make you two cup sizes bigger). It was a really col thought to me that I wouldn't need them anymore.
After all of this, I just waited until my big day came!
Pre-Op Appointment (2 Weeks Prior to Surgery)
Four days after I had my consultation, I was back in the officer for my pre-op appointment.
The staff had me fill out some more paperwork and copied two forms of ID and took the rest of my payment.
Soon, the patient coordination took me back into the consultation room. She sat down with my fiance and I and gave me what she called the "Patient's Bible". She said that we will cover everything that is in there, but it's a take home guide for me to refer to later.
This nice, professional, and easy to read soft cover bound booklet was very helpful and informative.
And... This booklet was seriously necessary!!
The topics it covered were:
- Preparing for surgery
- Medications to avoid
- Going to the surgery center and directions
- General surgical risks
- Specific surgical risks
- Anesthesia and other information
- Other risks
- Consent for surgery
- Post operative care - outpatient surgery
- Specific post operative instructions
- Longer tern post operative instructions
- As you heal
- Specifics as you heal
- Financial and cancellation polices
The patient coordinator then had me remove my top and put on the ugly looking bra. She brought in several different sizes of implants. She, again, had me put too different sizes in the bra without telling me what CC they were and asked me which one I liked best.
I picked my favorite and it was the same one I had picked at the consultation. It made me feel more confident that I was sure I knew what size I wanted to be post surgery. She noted it down on my chart and had me remove the bra and put on a robe.
We walked into the room where I had the 3d image taken at the consultation. The doctor met me in there and took a few pre-op photos of my chest. He then took some measurements of my breasts and told me that it would take 339cc implants to make my breasts int the masterpiece he wants them to be.
I was again very firm and said that I want a C cup, not a baby D. He was very patient and told me not to worry, they will not end up being too big.
Since I had done my research on him and his work, I believed him and had 100% confidence in him.
We again verified that I was going to have silicone implants placed under my pectoral muscles through the transaxillary (armpit) incision with the use of an endoscope, that I would have a pain pump.
The doctor went over all of the medications he was going to prescribe me and how to use them. I told him that anesthesia makes me throw up and narcotic pain killers also make me nauseous. He said he would prescribe me things to help with that as well and he'd let the anesthesiologist know about my sensitivity to anesthesia.
I was prescribed:
- Hibiclens (an over the counter antiseptic/antimicrobial surgical soap used to wash the skin/body the morning of the surgery)
- Emend (Aprepitant) 40mg capsule (to take 3 hours prior to surgery to help me not be nauseous when I wake up from anesthesia)
- Zofran (Ondansetron) 4mg tabs (to take after surgery to stop nausea if it were to get bad)
- Keflex (Cephalexin) 500mg capsules (antibiotic to take following surgery)
- Vicodin (Hydrocodone/Acetaminophen) 5-325mg tabs (Vicodin with acetaminophen for pain and swelling after surgery)
- Robaxin (Methocarbam) 500mg tabs (muscle relaxer for after surgery)
- Halcion (Triazolam) 0.25mg tabs (sleep aid for the night after surgery and as needed)
- Peri-Colace (a stool softener AND laxative to help with the constipation)
A hidden cost of getting a BA is the cost of prescription medication. If you do not have good prescription coverage, this could be expensive. And ALL of the medications your plastic surgeon prescribes ARE NECESSARY.
We went back to the consultation room for follow up questions and information.
Post-Op Blues:
The doctor reminded me that the day after surgery when he removes the bandages I need to understand it is not the final product.
He said the worst thing I can do it be expecting the final product and not less than 24 hour post-op swollen breasts. He also warned of the "post-op blues" where the patient becomes sad, depressed, upset, etc with having undergone surgery, the current result and how they feel.
He said some women feel this in varying degrees and some don't at all.
With all of that being said, all follow up questions answered, and feeling confident, I left the office with my surgery scheduled for June 26 at 3:30pm with an arrival time to the surgery center at 1:30pm.
I was excited and nervous!
Labels:
armpit incision,
Cephalexin,
consent,
doctor,
emend,
Halcion,
hidden cost,
Hydrocodone,
Keflex,
medications,
Methocarbam,
Ondansetron,
pain pump,
patient coordinator,
Post-Op Blues,
prescriptions,
risks
Subscribe to:
Posts (Atom)